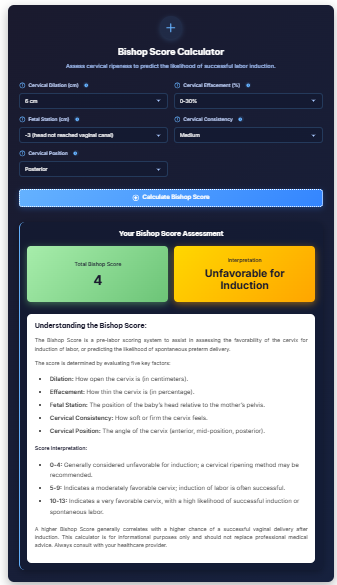
Bishop Score Calculator
Assess cervical ripeness to predict the likelihood of successful labor induction.
Wondering if your body is preparing for labor? Our Bishop Score Calculator helps healthcare providers and expectant parents assess cervical readiness for labor and predict the likelihood of successful labor induction. This clinical tool evaluates five key factors to generate a score between 0-13, providing valuable insights into whether your body is naturally preparing for childbirth or may need assistance. Understand this important obstetric assessment and how it guides decisions about induction timing and methods.
Start by tracking your pregnancy progress with our Pregnancy Calculator.
How to Use the Bishop Score Calculator
Our calculator helps you understand the clinical assessment process in three steps:
- Gather Cervical Examination Findings:
- Dilation: Cervical opening measured in centimeters (0-10 cm)
- Effacement: Cervical thinning measured as a percentage (0-100%)
- Station: Baby’s position relative to pelvic bones (-3 to +3)
- Cervical Consistency: Firm, medium, or soft assessment
- Cervical Position: Posterior, mid-position, or anterior
- Enter Your Assessment Data:
- Input measurements from your healthcare provider’s exam
- Select descriptors for consistency and position
- Note gestational age and any relevant medical factors
- Include any previous Bishop scores for comparison
- Interpret Your Results:
- View your total Bishop score (0-13 points)
- See likelihood of spontaneous labor within 24-48 hours
- Receive induction success probability assessment
- Get contextual interpretation based on your score
For accurate assessment, always rely on professional cervical exams by qualified healthcare providers.
Understanding the Bishop Score System
The Bishop Score evaluates five cervical characteristics to predict labor readiness:
Bishop Score Components and Scoring:
| Parameter | 0 Points | 1 Point | 2 Points | 3 Points |
| Dilation | 0 cm | 1-2 cm | 3-4 cm | ≥5 cm |
| Effacement | 0-30% | 40-50% | 60-70% | ≥80% |
| Station | -3 | -2 | -1/0 | +1/+2 |
| Position | Posterior | Mid-position | Anterior | – |
| Consistency | Firm | Medium | Soft | – |
Score Interpretation Guide:
| Total Score | Labor Probability | Induction Success | Typical Management |
| 0-4 | Unfavorable | Low (≤20%) | Cervical ripening needed |
| 5-7 | Intermediate | Moderate (50%) | May proceed with caution |
| 8-13 | Favorable | High (≥80%) | Likely successful induction |
Track your pregnancy timeline with our Due Date Calculator.
Why the Bishop Score Matters in Labor Assessment
This clinical tool provides crucial information for birth planning:
Labor Prediction:
- Identifies cervical readiness for spontaneous labor
- Predicts timing likelihood within next 24-48 hours
- Helps avoid unnecessary interventions when favorable
- Guides expectant management decisions
Induction Planning:
- Determines appropriate induction methods based on score
- Predicts induction-to-delivery time and success rates
- Helps avoid failed induction scenarios
- Guides medication choices for cervical ripening
Clinical Decision-Making:
- Supports evidence-based obstetric care
- Provides objective measurement of cervical status
- Helps timing of interventions for optimal outcomes
- Facilitates communication between providers and patients
Monitor your pregnancy health with our Pregnancy Weight Gain Calculator.
Factors Affecting Bishop Score Accuracy
Several variables can influence score interpretation:
Maternal Factors:
- Previous vaginal deliveries (scores often higher in multiparous women)
- Gestational age (scores naturally increase with advancing pregnancy)
- Maternal position during exam affecting station assessment
- Examiner experience and technique consistency
Clinical Considerations:
- Time of day (scores may vary throughout day)
- Recent activity (walking may temporarily improve scores)
- Hydration status affecting cervical characteristics
- Multiple exams potentially causing cervical changes
Medical Context:
- Indication for induction (medical vs. elective)
- Maternal medical conditions affecting cervical response
- Fetal factors including size and position
- Previous cervical procedures or surgeries
Use pregnancy tracking apps to monitor changes over time.
Natural Methods to Improve Bishop Score
While evidence varies, some approaches may help cervical readiness:
Medical Approaches:
- Membrane stripping (performed by healthcare provider)
- Prostaglandin medications for cervical ripening
- Foley catheter placement for mechanical dilation
- Misoprostol administration under medical supervision
Natural Techniques:
- Regular walking and upright positions
- Sexual intercourse (prostaglandins in semen)
- Nipple stimulation promoting oxytocin release
- Acupuncture or acupressure (limited evidence)
Lifestyle Factors:
- Adequate hydration maintaining cervical health
- Relaxation techniques reducing stress hormones
- Optimal nutrition supporting tissue health
- Proper rest conserving energy for labor
Important Note: Always consult your healthcare provider before attempting any methods to improve cervical readiness.
Track your contractions with our Contraction Timer Calculator.
Bishop Score in Special Situations
Unique considerations for specific circumstances:
Previous Cesarean Section:
- More conservative approach to induction
- Lower threshold for favorable score interpretation
- Different medication protocols for cervical ripening
- Enhanced monitoring during induction process
Premature Rupture of Membranes:
- Different interpretation of scores without amniotic fluid
- Time considerations due to infection risk
- Modified induction approaches based on score
- Antibiotic prophylaxis during waiting period
Medical Indications for Induction:
- Different thresholds for proceeding with induction
- More aggressive approaches despite unfavorable scores
- Continuous monitoring requirements
- Multidisciplinary decision-making process
Post-term Pregnancy:
- Generally more favorable scores with advancing gestation
- Still requires individual assessment of cervical readiness
- Consideration of fetal well-being in decision-making
- Discussion of risks/benefits of continued waiting vs. induction
Consider childbirth education classes to understand labor processes.
Common Bishop Score Misconceptions
Clarifying frequent misunderstandings:
Myth: A low score means I can’t go into labor naturally
Fact: The score predicts probability, not certainty. Spontaneous labor can still occur with low scores.
Myth: A high score guarantees easy labor
Fact: While favorable for induction, other factors like fetal position and maternal pelvis affect labor progress.
Myth: The score is the only factor in induction decisions
Fact: Clinical context, maternal preferences, and facility protocols all contribute to decisions.
Myth: I can accurately assess my own Bishop score
Fact: Proper assessment requires trained clinical examination and should not be attempted at home.
Use hospital bag checklists to prepare for potential induction.
Bishop Score Calculator FAQs
Q: At what gestational age is Bishop score typically assessed?
A: Usually around 39-41 weeks when considering induction, or earlier if medical indications exist.
Q: How often should Bishop score be reassessed during induction?
A: Typically every 12-24 hours during induction process to monitor progress and adjust methods.
Q: Does a Bishop score predict C-section risk?
A: Low scores are associated with higher C-section rates during induction, but many factors contribute to delivery outcomes.
Q: Can Bishop score change quickly?
A: Yes, cervical status can change rapidly, particularly in multiparous women or with cervical ripening agents.
Q: Is Bishop score used in spontaneous labor?
A: Primarily for induction planning, but may be assessed upon admission in spontaneous labor for progress prediction.
Next Steps After Bishop Score Assessment
Understanding your options based on score results:
Favorable Score (8-13):
- Likely successful induction with oxytocin or amniotomy
- Shorter anticipated induction-to-delivery time
- Lower intervention needs for cervical preparation
- Higher probability of vaginal delivery
Intermediate Score (5-7):
- May proceed with cautious induction
- Possible cervical ripening methods first
- Longer anticipated induction process
- Close monitoring for progress
Unfavorable Score (0-4):
- Cervical ripening recommended before induction
- Longer preparation period needed (possibly days)
- Higher intervention levels typically required
- Discussion of alternatives including continued waiting
Regardless of Score:
- Discuss findings thoroughly with your provider
- Understand risks and benefits of all options
- Consider personal preferences in decision-making
- Prepare emotionally for possible induction process
Consider labor support tools like birth balls and comfort measures.
Professional Perspectives on Bishop Score
How healthcare providers use this assessment:
Obstetrician Viewpoint:
- Evidence-based tool for induction planning
- Communication aid with patients about likelihoods
- Documentation of cervical status for medical records
- Guidance for method selection and sequencing
Midwifery Perspective:
- Part of holistic assessment of labor readiness
- Combined with other signs like energy changes, nesting
- Respect for natural timing when medically appropriate
- Shared decision-making tool with patients
Patient Experience:
- Understanding of where body stands in labor preparation
- Setting realistic expectations for induction process
- Participation in care decisions based on objective data
- Reduction of anxiety through information and planning
Use patient decision aids for induction choices.
Next Steps in Your Pregnancy Journey
Now that you understand Bishop score assessment:
- Discuss cervical status at your prenatal appointments
- Ask about your provider’s approach to induction decisions
- Learn about natural comfort measures for labor
- Prepare your birth preferences while remaining flexible
- Trust your healthcare team’s guidance combined with your instincts
Continue your pregnancy education with our Breastfeeding Calculator for postpartum planning.